AI in medical devices involves training computer models with data to replicate human intelligence, frequently employing techniques such as neural networks.
These AI models help predict diseases, analyze health data, improve treatments, and support diagnoses.
The combination of compliance, quality, and risk management has the potential to transform hospital management. AI is increasingly being incorporated into medical devices for a range of applications, and regulatory organizations, such as the FDA, ISO, and HIPAA, have introduced new guidelines.
Ensuring compliance allows us to harness AI’s vast potential to develop solutions that are safe, ethical, and impactful. AI is improving the personalization of healthcare delivery, optimizing hospital operations, and increasing healthcare accessibility through accurate decision-making tools.
The machine learning models are trained on carefully selected datasets and remain unchanged after training.
They do not undergo continuous training and do not access or retain any production data. Essential strategies for ensuring compliance in AI include:
- Conducting regular fairness assessments.
- Managing data quality with great care.
- Maintaining transparency in AI-based decision-making.
- Implementing strong privacy protections.
- Following clear ethical guidelines.
- Having oversight from diverse ethics committees.
These practices are crucial for the responsible development and use of AI in healthcare. The data sent to AI for processing is protected and secured when it leaves the hospital premises.
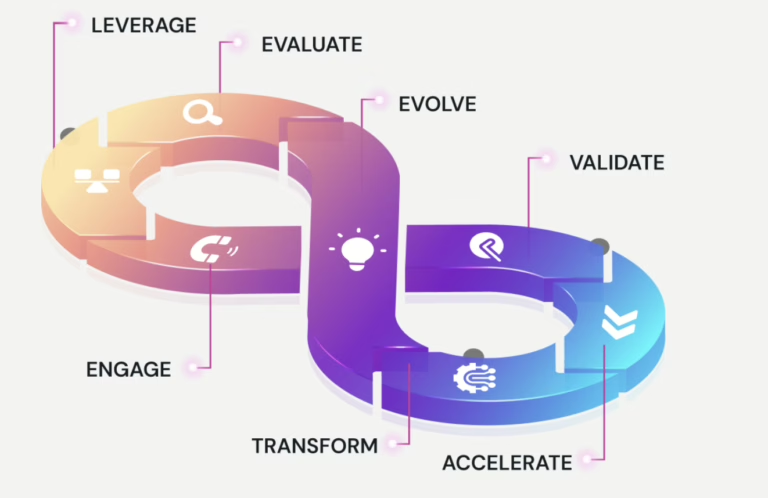
Maintaining AI-related compliance
It involves several key strategies and practices. Here’s an overview of how these concepts are addressed –
Fairness Check –
Regular testing ensures the AI avoids unfair group bias. Diverse data and system adjustments promote equal treatment. As the AI evolves, continuous fine-tuning maintains fairness.
Quality Data –
Meticulous data practices form the foundation of reliable AI. Detailed record-keeping and regular dataset updates ensure accuracy and minimize outdated biases.
Explaining AI Decisions –
Transparent algorithms aid understanding. User-friendly interfaces demonstrate AI reasoning, making it accessible to non-technical stakeholders.
Regulating policies –
These regulations validates that AI solutions are secure, perform well, and maintain patient privacy (PII &PHI).
Protecting Privacy –
Data minimization, strong encryption, and strict access controls safeguard information. Regular audits and updates address evolving threats and comply with privacy laws.
Playing by the Rules –
Clear ethical guidelines govern AI development. Regular assessments and third-party audits ensure compliance and ongoing team education keeps pace with evolving standards.
Ethics Watchdogs –
A diverse expert panel provides crucial ethical oversight. Regular meetings address concerns throughout the project lifecycle, and their recommendations shape responsible AI development and deployment.
Why Regulation of AI in Medical Devices?
Regulatory bodies like the FDA have started to approve medical devices that use AI more quickly, and this trend is expected to continue in 2024-2025. The deployment of AI in healthcare must adhere to stringent regulatory frameworks. Key regulations include the FDA’s guidelines for medical devices in the U.S., the General Data Protection Regulation (GDPR), and HIPAA. These regulations ensure that AI devices are safe and effective and respect patient privacy. Here’s how different countries regulate AI in medical devices:
- United States: The FDA ensures that medical devices, including those with AI, are safe and effective.
- European Union: The European Commission oversees medical device regulations like GDPR, MDR, etc.
- Ireland: The HPRA ensures medical devices are safe and of high quality.
- United Kingdom: The MHRA regulates AI-based medical devices, focusing on safety, quality, and effectiveness.
Addressing Risk Management and Safety
- Identifying and Mitigating Risks: AI algorithms can introduce unique risks, such as incorrect predictions due to data biases, hallucinations, or algorithmic errors. It is crucial to identify these risks early in the development process and implement strategies to mitigate them. This includes conducting thorough risk assessments and implementing testing protocols such as pen and vulnerability scans.
- Ensuring Patient Safety: Patient safety is paramount in healthcare. AI systems must be designed to prioritize safety, with built-in failed safety and the ability to override AI decisions when necessary. Regular updates and continuous monitoring are essential to ensure that the AI remains effective and safe over time.
Conclusion
AI has numerous applications in healthcare, but it also presents unique risks and challenges. Striking a balance between harnessing AI’s benefits and adhering to regulatory requirements is crucial. By aligning disciplines such as fairness in AI, data quality, explainability, privacy protection, ethical guidelines, and expert oversight, healthcare organizations can more effectively address the multifaceted challenges they face. AI, when properly regulated and refined, holds the promise not just to change healthcare but to transform lives. The key to realizing this potential lies in maintaining rigorous compliance practices that ensure AI solutions are fair, transparent, privacy-preserving, and ethically sound. As we look to the future, the integration of these compliance strategies will be fundamental in bringing the full possibilities of AI in healthcare to the forefront, creating a landscape where innovation and responsibility go hand in hand.