The Problem Isn’t Lack of Data
Every day, healthcare systems generate mountains of data, from electronic health records and lab results to imaging scans, wearables, and remote monitoring devices. But behind all that data are real people: a patient waiting for answers, a nurse struggling with multiple systems, a care team trying to make the best decision with incomplete information.
And here’s the hard truth: up to 80% of that data never gets used in clinical decision-making. It’s locked away in disconnected silos, making it harder – not easier, to deliver good care.
This fragmentation comes at a cost:
- $25 billion wasted annually in duplicate tests.
- 30% of preventable medical errors linked to missing or incomplete records.
- Value-based care contracts that underperform because providers can’t follow patients across networks.
For healthcare leaders, the message is clear: data needs to flow as freely as money does. Without it, even the best care strategies fall short.
Why Interoperability is no longer Optional?
Interoperability isn’t just a tech upgrade or a compliance checkbox, it’s a lifeline. It affects everything from clinical outcomes to operational efficiency to patient trust.
- For Providers: A complete, unified patient record means fewer readmissions, smoother care coordination, and better patient satisfaction.
- For Payers: Smarter data integration helps detect fraud, adjudicate claims in real time, and design preventative programs that actually reach people.
- For Pharma & Life Sciences: Connected data speeds up clinical trials and helps match real patients to real treatments faster.
- For Policymakers: Interoperable systems reduce national healthcare costs and improve access, especially for underserved communities.
This isn’t just an IT project. It’s a boardroom priority.
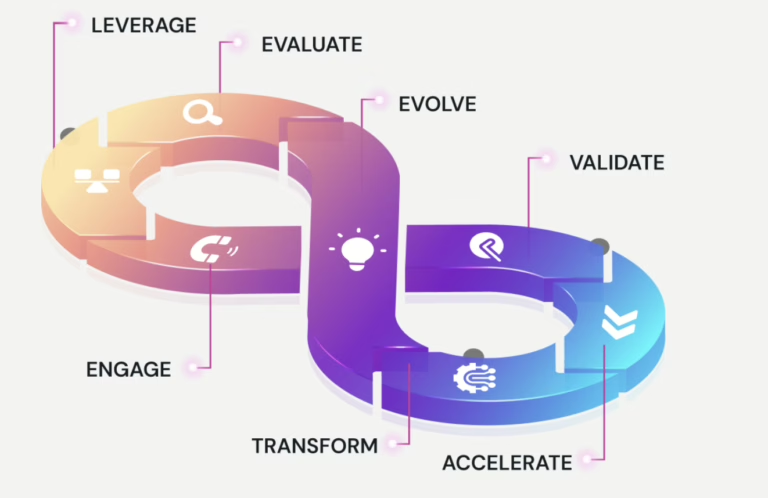
How AI Turns Data into Decisions?
Standards like FHIR and HL7 help move data between systems. But they don’t make it meaningful. That’s where AI comes in, adding the intelligence layer that makes data useful.
- Data Harmonization: AI cleans and connects messy data from different sources, creating a single, coherent view of each patient.
- NLP for Clinical Notes: AI reads physician notes, discharge summaries, and pathology reports—turning unstructured text into actionable insights.
- Entity Resolution: AI links fragmented identities, ensuring continuity of care.
- Contextual Intelligence: AI doesn’t just integrate, it interprets. For example, it can link abnormal ECG data from a wearable with a cardiologist’s note and a claims record to flag hospitalization risk before it happens.
What this looks like in Practice?
- Unified Care Dashboards Real-time, 360° patient views help care teams manage chronic conditions, coordinate across specialties, and personalize treatment.
- AI-Augmented Clinical Decision Support (CDS) Instead of generic alerts, clinicians get patient-specific recommendations, reducing burnout and improving outcomes.
- Population Health & Risk Stratification Payers and ACOs can forecast costs, identify high-risk individuals, and intervene early, before a crisis hits.
- Revenue & Operational Optimization CFOs can cut waste, streamline billing, and reinvest savings into better care delivery.
What Leaders need now?
- Cloud-Native Architectures: Scale across hospitals and networks.
- Federated Learning: Train AI models without compromising patient privacy.
- Explainable AI (XAI): Build clinician trust with transparent decision-making.
- Cybersecurity by Design: Embed HIPAA/GDPR compliance from the start, not as an afterthought.
What are the Challenges in Adoption?
- Culture & Adoption: Interoperability fails when it’s seen as “just tech.” Success requires clinical, operational, and financial alignment.
- ROI Justification: Boards want proof. Tie interoperability to reduced length of stay, improved HEDIS scores, and better Medical Loss Ratios.
- Collaborative Ecosystems: Providers, payers, device makers, and regulators must co-create. AI is the glue, but governance is the foundation.
What’s Next: From Interoperability to Intelligence
We’re entering a new era of autonomous care ecosystems:
- Virtual care agents that coordinate in real time.
- Predictive digital twins that guide proactive care.
- Health systems competing not on data volume, but on insight quality.
Final Word: It’s About People
AI-powered interoperability isn’t about machines – it’s about people. It’s about making every data point count toward better care, faster decisions, and healthier lives.
The question isn’t “Should we invest?” It’s: “How fast can we scale and how wisely can we lead?