From Compliance to Competitive Advantage
The shift in healthcare isn’t just about meeting requirements anymore—it’s about using performance as a lever for transformation. As the National Committee for Quality Assurance (NCQA) redefines quality evaluation through HEDIS® ECDS (Electronic Clinical Data Systems), Health Equity, and digital measurement reporting, a new data mandate emerges: Make data the driver of performance—not just its recorder.
Organizations that once focused solely on reporting compliance are now building performance-first data strategies—putting outcomes at the center and using data to drive, predict, and optimize those outcomes.
Understanding NCQA’s Roadmap: The Three Fronts of Transformation
1. Digital Quality Measures (dQMs) & ECDS NCQA is evolving from static, retrospective reporting to real-time, electronic measurement.
- ECDS allows organizations to report HEDIS measures using multiple digital sources, including EMRs, case management, and lab systems.
- Goal: More accurate, timely, and comprehensive performance measurement.
2. Health Equity and Stratification Equity is no longer a parallel priority—it’s central.
- NCQA now encourages stratification of quality metrics by race, ethnicity, language, SDOH indicators.
- This requires cleaner, more complete member-level data and alignment with CMS’s Health Equity Index.
3. Interoperability and Data Quality NCQA stresses the need for structured, standardized, and sharable data via FHIR and APIs.
- The 2025-2027 roadmap includes incentives for organizations to move toward seamless clinical and payer data integration.
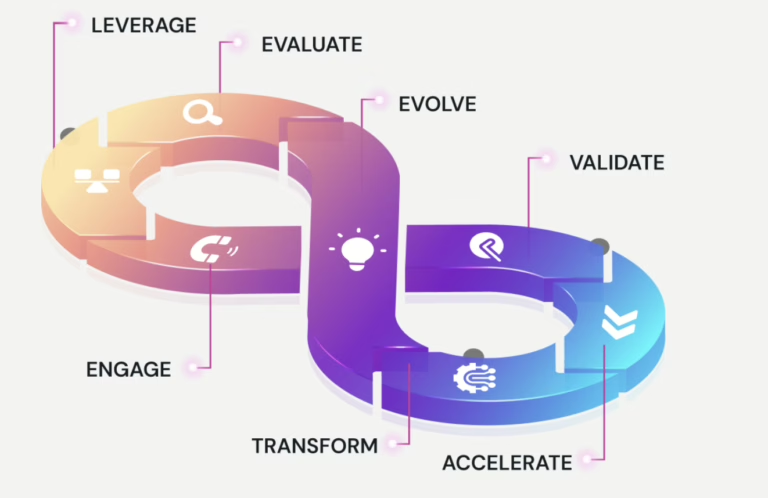
Performance-First Data Strategy: What It Really Meana
Instead of just collecting data to report outcomes, a performance-first strategy –
- Integrates clinical, financial, and behavioral data to predict gaps in care.
- Builds real-time dashboards tied to HEDIS and Stars measures.
- Prioritizes patient-level performance insights over aggregate reporting.
- Uses AI and predictive modeling to intervene before a care gap becomes a metric failure.
This strategy aligns deeply with NCQA’s forward-looking initiatives. Let’s break it down:
How the Alignment Works: NCQA Roadmap x Performance-First Strategy?

Aligning for Success
For example a Regional Payer (Medicare + Medicaid) faces this challenge – Low Stars scores, poor HEDIS compliance, and limited equity stratification
The Solution can be –
· Building centralized data warehouse (FHIR-ready)
· Applying machine learning to predict non-compliance 90 days in advance
· Developing provider dashboards showing real-time measure performance and social risk indicators
Possible outcomes –
· Stars scores improvement by 1 full point in 12 months
· Most of measures reported via ECDS
· 2x engagement in care gaps among Black and Hispanic populations
Key Capabilities for Performance-First Strategy
- Data Enrichment: SDOH APIs, NLP for unstructured notes, member verification
- AI-Driven Insights: Predictive care gaps, stratified risk modeling
- Smart Reporting: Measure engines aligned to NCQA’s digital specs
- Equity Audits: Real-time equity dashboards, DEI stratification frameworks
- Governance: Cross-department data councils with NCQA reporting responsibility
Strategic Compliance is the New Competitive Advantage
Those who treat NCQA’s roadmap as a strategic opportunity, not a burden, will outperform. Performance-first data strategies aren’t just better at reporting—they’re better at caring.
The organizations that will lead in the next phase of value-based care are those that optimize today’s data to perform tomorrow’s outcomes.
Schedule your free consultation – “How to Align Your Data Strategy with NCQA’s Roadmap”