What if patients start paying hospitals based on their health outcomes? This “too good to be true” healthcare model is called Value-Based Care, or VBC. Although this sounds like a patient-centric approach (which it is), the model also benefits healthcare providers.
Michael Porter and Elizabeth Olmsted Teisberg first coined the term “Value-Based Health Care” in their book Redefining Health Care. In less than a couple of decades, VBC has driven the healthcare industry into an era of near-perfect efficiency and accuracy.
But why is Value-Based Care so crucial for the healthcare sector?
Healthcare costs are soaring. In this scenario, VBC offers a sustainable solution that improves patient health while reducing overall expenses.
In other words, VBC puts health outcomes at the “heart” of healthcare delivery.
One critical aspect of successfully implementing VBC is the seamless integration of diagnostic data with healthcare records. It’s a great way to ensure accurate, timely, and efficient diagnoses.
However, despite advances in medical technology, diagnostically connecting data from disparate sources remains a challenge. This is because most healthcare systems still operate in silos.
Moreover, crucial diagnostic information often doesn’t flow smoothly across the entire care continuum. To bridge this gap, healthcare providers are adopting a new approach—a data-driven diagnosis that leads to precise and personalized medicine.
In this blog, we’ll explore how value-based care connects diagnostic data with patient records and discuss the challenges and solutions involved in this process.
What is Value-Based Care?
At its core, Value-Based Care (VBC) is a healthcare delivery model which validates that the hospitals and physicians are paid only based on patient health outcomes. This is in stark contrast to the fee-for-service (FFS) model, where providers are compensated for each service.
In other words, VBC emphasizes the quality of healthcare rather than the quantity.
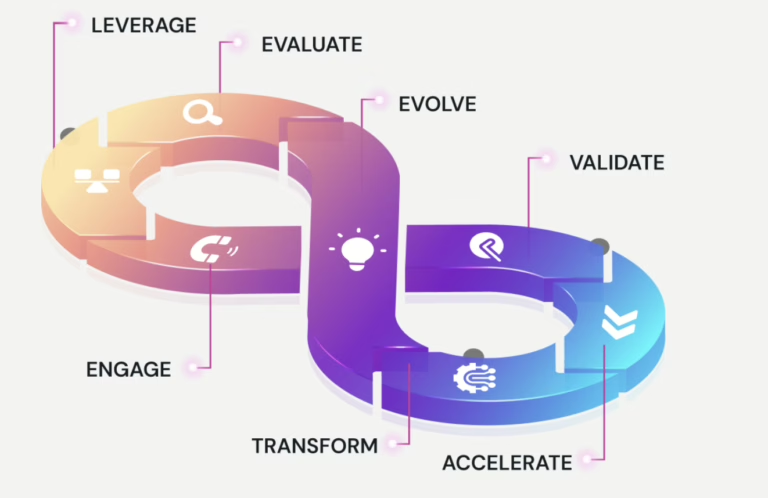
Let’s look at some of the key elements of Value-Based Care:
Preventive Care: As wise people say, “Prevention is better than cure”. The VBC model of healthcare delivery promotes early interventions to prevent chronic conditions. Preventive healthcare results in:
- Fewer hospital admissions
- Better control of rising costs
- Improved long-term health outcomes for patients
Care Coordination: Care coordination means all healthcare providers (from primary care doctors to specialists) involved in a patient’s care work are in synergy. This holistic approach:
- Reduces treatment delays
- Prevents redundant procedures
- Offers more cohesive and personalized care to the patient
Data-Driven Decisions: Data and analytics are the fuel that powers value-based care in healthcare. Data-driven diagnosis enables doctors and paramedics to make evidence-based, informed decisions.
Subsequently, patients get more personalized treatment plans, and there is a better use of medical resources.
Challenges in Connecting Data and Diagnosis in VBC
Despite its many benefits, implementing value-based Care in healthcare is not without its challenges. Many healthcare systems still operate under the traditional fee-for-service model.
Moreover, transitioning to VBC requires a cultural shift as well as significant technological upgrades.
And, despite the digital evolution, a lot of healthcare systems still operate in silos. Consequently, the diagnostic data from labs, imaging centers, and patient records often do not converge in real-time.
This fragmentation slows down the diagnostic process and can lead to delayed treatment or misdiagnoses, which in turn negatively impacts patient outcomes.
In addition, the lack of interoperability between healthcare providers, hospitals, and diagnostic facilities creates barriers to seamless data sharing.
Healthcare organizations must overcome these obstacles by adopting a digital-first approach to Care. Data-driven diagnosis can help solve some of the major challenges in the widespread adoption of Value-Based Healthcare. Let’s explore it in further detail.
Benefits of Diagnostically Connected Data in Value-Based Care
Connecting data and diagnosis in value-based Care has transformative benefits for patients, providers, and the healthcare system overall:
1. Enhanced Clinical Decision-Making – Imagine you’re a doctor faced with a patient juggling multiple chronic conditions. Having all diagnostic data at your fingertips changes the game! You see their lab results, imaging scans, and medical history in one seamless view. Instantly, you connect the dots and create a plan that tackles everything—diabetes, hypertension, and that nagging kidney issue—together. No delays, no missed details, just targeted Care. With this kind of connected data, you’re not just treating symptoms; you’re transforming lives. That’s the power of smarter decision-making.
2. Increased Patient Engagement – By connecting diagnostic data to diagnoses, patients gain a clearer understanding of their health journey. Patients who can see the connection between their diagnostic results and their prescribed treatments are more likely to engage with their care plans and adhere to medical advice, which is particularly valuable for managing chronic conditions.
3. Proactive and Preventive Care – Value-based care models emphasize prevention and early intervention. Connected data allows providers to detect early warning signs and intervene before conditions worsen. In preventive care, access to historical and real-time diagnostic data enables providers to recommend lifestyle changes, medications, or therapies that mitigate risks and reduce the need for costly interventions down the line.
4. Reduction in Unnecessary Testing – A connected approach reduces the need for duplicate tests and procedures. When diagnostic data is integrated and accessible across providers, unnecessary testing can be minimized, resulting in cost savings and a better patient experience.
5. Streamlined Care Coordination – Coordinated Care is critical in a value-based care environment, particularly for patients with complex health needs. Connected diagnostic data enables smoother handoffs and better communication among providers, fostering a team-based approach where each healthcare professional has access to the same critical information about the patient.
Technological Enablers for Connecting Data and Diagnosis
To achieve diagnostically connected Care, healthcare systems require the proper technological foundation. Several advancements are driving this shift:
1. Electronic Health Records (EHRs)
Modern EHRs play a significant role in centralizing patient data, including diagnostic information. However, many EHRs still need to be designed with fragmented data management, making it challenging to integrate diagnostic data fully. Improved EHR interoperability, where systems can share information seamlessly, is essential for supporting connected diagnostic and diagnostic-driven care.
2. Artificial Intelligence and Machine Learning
AI and machine learning are tools that can analyze vast amounts of diagnostic data to identify patterns and predict outcomes. These technologies helps with the clear understanding of complex cases, support early diagnosis, and assist in personalizing treatment recommendations. For example, machine learning algorithms can analyze imaging data for early signs of conditions like cancer, alerting clinicians to potential issues before symptoms develop.
3. Data Integration Platforms
Data integration platforms bring together data from various sources, such as lab systems, imaging centers, and clinical data repositories, creating a unified view of patient information. These platforms facilitate interoperability, ensuring that data flows seamlessly across systems and is available when needed.
4. Patient-Reported Outcome Measures (PROMs)
PROMs are data points gathered directly from patients, often through surveys or mobile apps. They provide additional context to diagnostic data, offering insights into the patient’s quality of life, mental health, and satisfaction with their care. When integrated with diagnostic data, PROMs contribute to a holistic view of the patient’s health status and response to treatment.
A New Approach: Data-Driven Diagnosis & Healthcare
This is the age of big data and artificial intelligence (AI) in medical diagnostics. Today, healthcare providers can analyse mountains of diagnostic data efficiently. Moreover, tech experts are leveraging advanced machine learning (ML) models to enhance predictive analytics in healthcare and medicine.
Additionally, integration of diagnosis data, such as lab results or imaging scans, with electronic health records (EHRs) can solve the interoperability issue in VBC implementation.
Moreover, AI in healthcare has made it easier to identify patterns, predict patient risk, and suggest precise treatment plans.
For example, cross-referencing a patient’s health history with a current test can flag potential issues before they escalate. This results in earlier interventions that can save lives and reduce healthcare costs.
The Future of Diagnostic Data Integration in Value-Based Care
The future of VBC will depend on how effectively data can be harnessed to inform diagnosis. Technologies, like wearable devices and remote monitoring tools, helps in the collection of continuous streams of patient data.
However, interoperability and data fluidity will be the key to the widespread adoption of Value-Based Care. Big data analytics and AI can help make the best use of the data from health monitoring devices.
This data, when integrated with other diagnoses, can help design personalized treatment plans. Personalized medicine can drastically improve the efficacy of medicines and reduce the costs incurred in treatment.
In conclusion, seamless data integration and advanced analytics in medical diagnosis will make VBC a win-win delivery model for both patients and healthcare providers.