AI agents are diligently working in the background to assist clinicians, reduce administrative burdens, and improve patient monitoring. These AI tools have become taskmasters – they schedule, document, calculate, and observe.
But as technology matures, so does its role in healthcare. A quiet revolution is underway. AI in virtual care is no longer just passive or reactive—it’s becoming active, empathetic, and personalized.
We are witnessing the emergence of AI as a health advocate- one that understands not just the data, but the person behind it.
AI Agents – From Silent Guardian to Active Advocate
Traditionally, AI agents worked behind the scenes—optimizing appointments, parsing through vast amounts of clinical data, monitoring vitals, and generating alerts. They were incredibly useful for improving operational efficiency.
But today’s AI is crossing that threshold. It’s becoming more emotionally intelligent, context-aware, and capable of initiating meaningful engagement.
Example – Imagine an AI agent monitoring a diabetic patient. Not only does it remind them to take insulin—it changes its tone when the patient is stressed, detected via voice modulation or wearable signals. It follows up with motivational nudges, offers breathing exercises, or prompts a tele-consult when needed.
Or consider a patient struggling with post-operative depression. An AI system might flag emotional cues from typed messages or tone in a telehealth session and proactively notify the physician with an well-being summary.
In this new paradigm, AI isn’t just executing instructions—it’s making informed, human-centered decisions.
The Technology Behind the Transformation
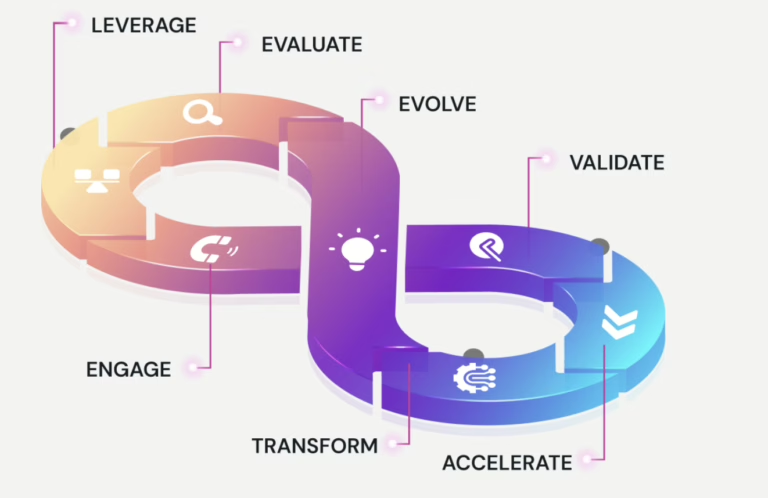
This leap from passive assistance to proactive advocacy is enabled by a convergence of advanced technologies –
Emotional AI (Affective Computing) – AI is now capable of reading micro-expressions, analyzing voice stress patterns, and even interpreting keystroke dynamics to understand how a person feels. It’s the beginning of empathetic computing.
Natural Language Processing (NLP) – Sophisticated NLP allows AI to comprehend and engage in human conversations. It can analyze sentiment, detect anxiety or hesitation in speech, and respond contextually during patient interactions.
Predictive Analytics – By integrating data from wearables, EHRs, lifestyle inputs, and even social determinants of health, predictive AI can forecast health deterioration, medication adherence issues, or mental health concerns—before they become critical.
Personalized Recommendation Engines – AI agents can now tailor care paths dynamically. For instance, if a patient has missed a few exercise sessions and is also experiencing poor sleep, the AI can tweak the wellness plan, add motivational content, or flag the case for clinician follow-up.
Benefits Across the Board
The impact of this shift is not isolated—it ripples across the entire healthcare ecosystem:
For Patients –
- Receive care that’s more timely, contextual, and empathetic.
- Benefit from interventions that align with their mood, behavior, and preferences.
- Feel heard, supported, and nudged—not just managed.
For Clinicians –
- Offload repetitive tasks like data entry, scheduling, and documentation.
- Receive real-time summaries of patient behavior and emotional states.
- Spend more time focusing on meaningful clinical decisions and patient relationships.
For Healthcare Systems –
- Improve patient outcomes and satisfaction scores.
- Optimize resource allocation and reduce unnecessary admissions.
- Leverage AI insights for population health management and early interventions.
Ethical and Practical Considerations
While the potential is transformative, this evolution is not without its challenges.
Data Privacy – As AI collects more intimate and emotional data, robust frameworks must ensure confidentiality, informed consent, and ethical data usage.
Bias and Equity – If AI models are trained on biased data, they risk reinforcing health disparities. Diverse and inclusive datasets are essential for equitable AI-driven care.
Transparency and Trust – Clinicians and patients alike need to understand how an AI arrived at a recommendation. Explainability is critical for adoption and trust.
Key Question – Can a doctor trust an AI’s emotional read of a patient? And can a patient trust that their data won’t be used against them?
What’s Next?
We’re entering a new era where AI is not just a backend tool—it’s a partner in care.
AI-driven Health Companions – Think of them as virtual nurses—checking in daily, offering reminders, answering queries, and escalating red flags.
Dynamic Care Plans – Care paths that adjust not just to vitals, but to mood shifts, behavioral trends, and life changes.
Regulatory Innovation – Expect evolving frameworks from health bodies and governments to govern responsible AI deployment with ethical safeguards.
Conclusion
AI in virtual care is evolving from a digital assistant into a true health advocate. It’s no longer just about automation or efficiency—it’s about empathy, trust, and meaningful engagement.
By bridging technology and human understanding, AI agents are helping reshape the future of healthcare—one personalized interaction at a time.
This is just the beginning.
Stay tuned – In our next articles, we’ll understand real-world case studies and tools that are making AI advocacy a reality across hospitals, clinics, and homes.