Interoperability in Electronic Health Records (EHRs) has been a buzzword for over a decade, yet we’re still chasing its full potential. Despite billions in digital health investments and mandates like the 21st Century Cures Act, most clinicians still wrestle with systems that don’t talk to each other. The result? Burned-out doctors, medical errors, and fragmented patient care.
According to a recent KLAS report, over 70% of clinicians express frustration with external data integration. They’re digging through duplicate records, outdated test results, and siloed systems while trying to deliver timely care. That’s not just inefficient but dangerous. Medical errors caused by poor data access rank among the top 10 causes of death in the U.S.
So, what’s holding us back?
We’re stuck between legacy systems that can’t evolve and modern standards that aren’t consistently applied. And we’re asking healthcare providers to fix it themselves — with limited budgets, tight timelines, and no tech army. It’s like giving them a spaceship without a manual and expecting a perfect launch.
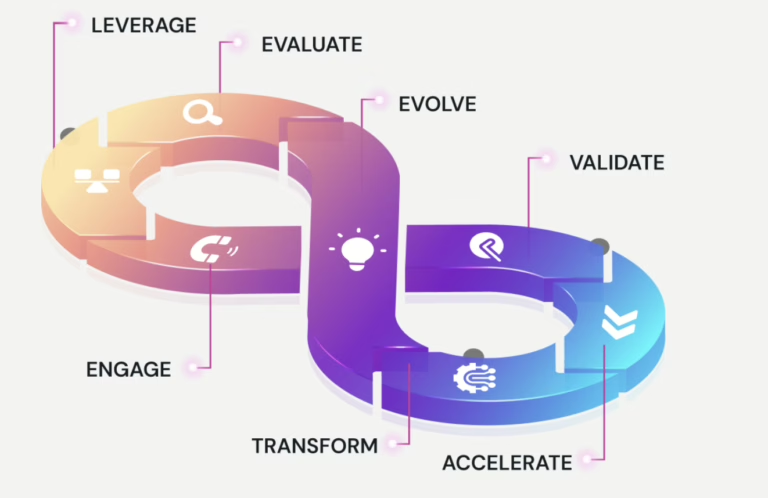
But there’s hope. AI, middleware, and no-code platforms are turning the tide. Tools are simplifying integrations without code, making interoperability a reality. The convergence of API-first design, machine learning, and intuitive platforms finally makes seamless, secure data exchange within reach.
This whitepaper cuts through the noise. It explores why interoperability still fails, what needs to change, and how we can finally bridge the gaps – for clinicians, patients, and the future of care.