How can a health insurance company gain a strategic advantage by measuring, analyzing, and acting upon quality measures to keep their members healthy.
The Institute of Medicine (IOM) defines the following six goals for the health care system.
- Safe: Avoiding harm to patients from the care intended to help them.
- Effective: Providing services based on scientific knowledge to all who could benefit and refraining from providing services to those not likely to help (avoiding underuse and misuse, respectively).
- Patient-centered: Providing care respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions.
- Timely: Reducing waits and sometimes harmful delays for those who receive and those who give care.
- Efficient: Avoiding waste, including waste of equipment, supplies, ideas, and energy.
- Equitable: Providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.
To achieve these goals, the care and outcomes have to be monitored, quantified and improved using a set of measures. With the focus of the healthcare industry shifting from pay-for-service to pay-for-value, measuring healthcare quality has become extremely important. The measures used to assess and compare the quality of health care organizations are classified into structural, process, or outcome measures. (Reference: Agency for Healthcare Research and Quality)
Structural Measures
Structural measures give consumers a sense of a health care plan’s capacity, systems, and processes to provide high-quality care. For example:
- How many health care providers within the plan use electronic medical records or medication order entry systems.
- The number or proportion of board-certified physicians enrolled in the plan.
- The ratio of providers to total plan members in a given geography.
Process Measures
Process measures indicate what a plan does to maintain or improve health or block progress towards chronic illness for healthy people or those diagnosed with a health care condition. These measures involve ensuring that providers follow clinical protocols for cancer screenings, diabetes management, childhood immunization status, asthma medication management, heart attack treatment, mental healthcare, flu shots, high blood pressure treatment, etc. For example:
- The percentage of people receiving preventive services (such as mammograms or immunizations).
- The percentage of people with diabetes who had their blood sugar tested and controlled.
Process measures can inform consumers about the medical care they may expect to receive for a given condition or disease and can contribute to improving health outcomes. Most health care quality measures used for public reporting are process measures.
Outcome Measures
Outcome measures reflect the impact of the health care service or intervention on the health status of patients. For example:
- The percentage of patients who died due to surgery (surgical mortality rates).
- The rate of surgical complications or hospital-acquired infections.
Outcome measures may seem to represent the “gold standard” in measuring quality, but an outcome results from numerous factors, many beyond providers’ control. Risk-adjustment methods — mathematical models that correct for differing characteristics within a population, such as patient health status — can help account for these factors. However, the science of risk adjustment is still evolving. Experts acknowledge that better risk-adjustment methods are needed to minimize the reporting of misleading or even inaccurate information about health care quality.
Health Plan Quality Measures
In the context of insurance companies and health plans, quality measures combine clinical quality (doing the right thing, at the right time, to the right patient) and the health plan member’s experiences with care. Here are some examples of health plan quality measures that are useful.
Patient Safety Measures
- The percentage of health plan members on persistent prescription medications who are monitored.
- The percentage of elderly health plan members diagnosed with certain chronic conditions receiving contraindicated medications.
Effectiveness Measures
- The percentage of health plan members receiving recommended care (i.e., a treatment or an assessment) for a specific health condition. Today’s measures address diabetes, cardiovascular disease, musculoskeletal disorders, respiratory conditions, or behavioral health.
- The percentage of health plan members receiving preventive care such as immunizations, flu shots, smoking cessation counseling, and obesity counseling.
- The percentage of health plan members receiving screenings for cancers, lead, glaucoma, Chlamydia, and obesity.
Patient-Centeredness Measures
- Health plan members report on the care and service they received from the health plan and the doctors and nurses associated with it.
- Rates of health plan member complaints or appeals over coverage decisions.
Timeliness Measures
- The percentage of health plan members who had an annual visit with primary care or dental practitioner.
- The percentage of pregnant women receiving prenatal care during the first trimester or postpartum care after delivery.
Descriptive Measures
- Percentage of board-certified physicians.
- Status of health plan accreditation.
- The number of health plan members.
Data Sources for Health Plan Quality Measures
Depending on the measure, data can be collected from different sources, including medical records, patient surveys, and administrative databases used to pay bills or manage care. Each of these sources may have other primary purposes, so there are advantages and challenges when they are used for quality measurement and reporting.
Administrative Data
In the course of providing and paying for care, organizations generate administrative data on the characteristics of the population they serve and their use of services and charges for those services, often at the level of individual users. The data is gathered from claims, encounters, enrollment, and providers systems. Common data elements include the type of service, number of units (e.g., days of service), diagnosis and procedure codes for clinical services, service location, amount billed, and the amount reimbursed. Claims data consists of the billing codes that physicians, pharmacies, hospitals, and other health care providers submit to payers (e.g., insurance companies, Medicare). This data benefits from following a relatively consistent and structured format and using a standard set of pre-established codes that describe specific diagnoses, procedures, and drugs. Additionally, since all health care providers want to be paid for their services, nearly every encounter that a patient has with the medical system leads to the generation of a claim, creating an abundant and standardized source of patient information.
Claims data also include essential details about medications – Every fill/refill of a prescription, complete with the date of that event, information about the dispensed drug, the amount of drug that was dispensed, and the number of days that the medication should last. Any services provided by a provider not using an EMR will fail to be reflected in EMR data. The claims data, however, will contain evidence of them because all of these services need to be reimbursed, only through claims data that a holistic view of the patient’s interactions with the health care system can be seen.
Advantages of Administrative Data
- Available electronically.
- Less expensive than obtaining medical record data.
- Available for an entire population of patients and across payers.
- Relatively uniform (and improving) coding systems and practices.
Challenges of Administrative Data
- Limited clinical information.
- Questionable accuracy for public reporting because the primary purpose is billing.
- Completeness.
- Timeliness.
Electronic Medical Record (EMR) Data
An Electronic Medical Record (EMR) documents a patient’s medical history and care. EMR is a much richer dataset than is claims data. At its heart, claims data is designed to hold only those pieces of information that are required to facilitate payment by an insurance company: what service was provided, the diagnosis; who was the service provider, how much money is owed for that service. However, the EMR contains a lot more detail:
- Vital signs and lab results (as noted in the CKD and high blood pressure examples)
- Information from the patient:
- Habits: smoking and alcohol use
- List of non-prescription drugs (which don’t appear in claims data) taken by the patient, such as aspirin
- Results of surveys given to the patient: i.e., PHQ-9 is often used for depression monitoring or screening i.e., Asthma Control Test (ACT), which is used to monitor asthma severity i.e., SF-36 which measures the patient quality of life
- The information recorded by nurses, pharmacists, and other team members involved in the case or disease management
Advantages of Medical Records
- Rich in clinical detail.
- Viewed by providers as credible.
Challenges of Medical Records
- The cost, complexity, and time required to compile data when patients receive services across different sites, mainly if a different record format is used.
- The current use of paper for most records means that trained medical coders must manually abstract information using stare-and-compare or automatic extraction tools.
Patient Surveys
Survey instruments capture self-reported information from patients about their health care experiences. Aspects covered include reports on the care, service, or treatment received and perceptions of care outcomes. Surveys are typically administered to a sample of patients by mail, telephone, or Internet.
Advantages of Patient Surveys
- Captures types of information for which patients are the best source.
- Well-established methods for survey design and administration.
- Easy for consumers to understand and relate to survey results.
Challenges of Patient Surveys
- Cost of survey administration.
- Possibly misleading results if questions are worded poorly, survey administration procedures are not standardized, the population sampled is not representative of the population (sampling bias), or the population is not represented in the responses (response bias).
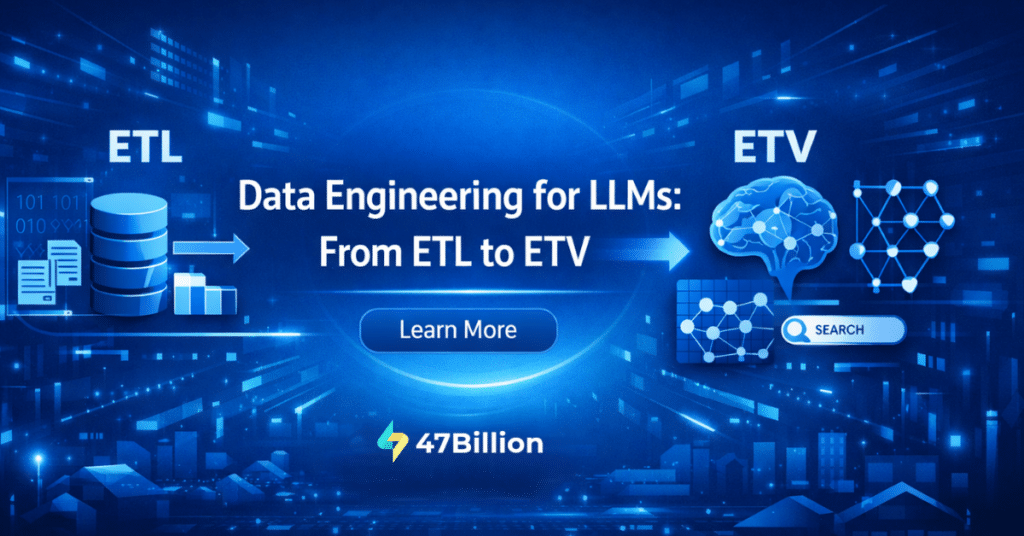
Neither claims data, EMR data, or patient surveys alone can provide a complete, accurate, and timely view of a person’s health status. The future of health data analysis will depend on integrating all data sources and leveraging the strengths of each.
HEDIS Health Plan Quality Measurements
The Healthcare Effectiveness Data and Information Set (HEDIS) is a tool used by more than 90 percent of America’s health plans to measure performance on critical dimensions of care and service. Altogether, HEDIS consists of 94 measures of process, structure, and outcomes across seven domains of care. Because so many plans collect HEDIS data, and because the measures are so specifically defined, HEDIS makes it possible to compare the performance of health plans on an “apples-to-apples” basis. HEDIS measures promote accountability, streamline measurement and evaluate provider performance. HEDIS scores are regarded as highly credible because an NCQA-approved auditing firm must validate results. Also, an NCQA-approved external survey organization must administer the CAHPS survey when it is part of a health plan’s HEDIS submission to NCQA.
Conclusion
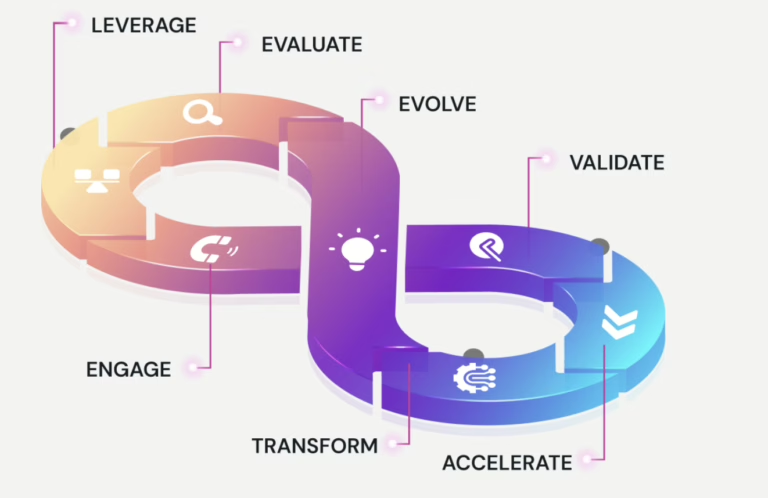
Healthcare plans are transforming from a traditional fee-for-service model to a population health model. The focus is to measure healthcare quality using standards and using them in transformation by aligning all players in the health care system to focus on a population’s overall health and long-term well-being. The quality measures have a significant role in the healthcare industry regarding closing gaps in care and decreasing the use of costly acute care through preventive services. By placing a greater focus on value-based care and quality improvement across healthcare organizations, quality measures are critical in helping providers achieve these goals.
Reference: HEDIS Measures
Prevention and Screening
- Adult BMI Assessment
- Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents
- Childhood Immunization Status
- Immunizations for Adolescents
- Lead Screening in Children
- Breast Cancer Screening
- Cervical Cancer Screening
- Colorectal Cancer Screening
- Chlamydia Screening in Women
- Care for Older Adults
Respiratory Conditions
- Appropriate Testing for Children With Pharyngitis
- Use of Spirometry Testing in the Assessment and Diagnosis of COPD
- Pharmacotherapy Management of COPD Exacerbation
- Medication Management for People With Asthma
- Asthma Medication Ratio
Cardiovascular Conditions
- Controlling High Blood Pressure
- Persistence of Beta-Blocker Treatment After a Heart Attack
- Statin Therapy for Patients With Cardiovascular Disease
Diabetes
- Comprehensive Diabetes Care
- Statin Therapy for Patients With Diabetes
Musculoskeletal Conditions
- Disease-Modifying Anti-Rheumatic Drug Therapy for Rheumatoid Arthritis
- Osteoporosis Management in Women Who Had a Fracture
Behavioral Health
- Antidepressant Medication Management
- Follow-Up Care for Children Prescribed ADHD Medication
- Follow-Up After Hospitalization for Mental Illness
- Follow-Up After Emergency Department Visit for Mental Illness
- Follow-Up After Emergency Department Visit for Alcohol and Other Drug Abuse or Dependence
- Diabetes Screening for People With Schizophrenia or Bipolar Disorder Who Are Using Antipsychotic Medications
- Diabetes Monitoring for People With Diabetes and Schizophrenia
- Cardiovascular Monitoring for People With Cardiovascular Disease and Schizophrenia
- Adherence to Antipsychotic Medications for Individuals With Schizophrenia
- Metabolic Monitoring for Children and Adolescents on Antipsychotics
Medication Management and Care Coordination
- Annual Monitoring for Patients on Persistent Medications
- Medication Reconciliation Post-Discharge
- Transitions of Care
- Follow-Up After Emergency Department Visit for People With High-Risk Multiple Chronic Conditions
Overuse/Appropriateness
- Non-Recommended Cervical Cancer Screening in Adolescent Females
- Non-Recommended PSA-Based Screening in Older Men
- Appropriate Treatment for Children With Upper Respiratory Infection
- Avoidance of Antibiotic Treatment in Adults With Acute Bronchitis
- Use of Imaging Studies for Low Back Pain
- Use of Multiple Concurrent Antipsychotics in Children and Adolescents
- Potentially Harmful Drug-Disease Interactions in the Elderly
- Use of High-Risk Medications in the Elderly
- Use of Opioids at High Dosage
- Use of Opioids from Multiple Providers
- Measures Collected Through the Medicare Health Outcomes Survey
- Medicare Health Outcomes Survey
- Fall Risk Management
- Management of Urinary Incontinence in Older Adults
- Osteoporosis Testing in Older Women
- Physical Activity in Older Adults
Measures Collected Through the CAHPS Health Plan Survey
- Flu Vaccinations for Adults Ages 18–64
- Flu Vaccinations for Adults Ages 65 and Older
- Medical Assistance With Smoking and Tobacco Use Cessation
- Pneumococcal Vaccination Status for Older Adults
Access/Availability of Care
- Guidelines for Access/Availability of Care Measures
- Adults’ Access to Preventive/Ambulatory Health Services
- Children and Adolescents’ Access to Primary Care Practitioners
- Annual Dental Visit
- Initiation and Engagement of Alcohol and Other Drug Abuse or Dependence Treatment
- Prenatal and Postpartum Care
- Use of First-Line Psychosocial Care for Children and Adolescents on Antipsychotics
Experience of Care
- CAHPS Health Plan Survey 5.0H, Adult Version
- CAHPS Health Plan Survey 5.0H, Child Version
- Children With Chronic Conditions
Utilization and Risk-Adjusted Utilization
- Guidelines for Utilization Measures
- Frequency of Ongoing Prenatal Care
- W15 Well-Child Visits in the First 15 Months of Life
- Well-Child Visits in the Third, Fourth, Fifth, and Sixth Years of Life
- Adolescent Well-Care Visits
- Frequency of Selected Procedures0
- Ambulatory Care
- Inpatient Utilization — General Hospital/Acute Care
- Identification of Alcohol and Other Drug Services
- MPT Mental Health Utilization
- Antibiotic Utilization
- Standardized Healthcare-Associated Infection Ratio
- Guidelines for Risk-Adjusted Utilization Measures
- Plan All-Cause Readmissions
- Inpatient Hospital Utilization
- Emergency Department Utilization
- Hospitalization for Potentially Preventable Complications
Relative Resource Use
- Guidelines for Relative Resource Use Measures
- Relative Resource Use for People With Diabetes
- RCA Relative Resource Use for People With Cardiovascular Conditions
- Relative Resource Use for People With Hypertension
- Relative Resource Use for People With COPD
- Relative Resource Use for People With Asthma
Health Plan Descriptive Information
- Board Certification
- Enrollment by Product Line
- Enrollment by State0
- Language Diversity of Membership
- Race/Ethnicity Diversity of Membership
- Total Membership
Measures Collected Using Electronic Clinical Data Systems
- Guidelines for Measures Collected Using Electronic Clinical Data Systems
- Depression Screening and Follow-Up for Adolescents and Adults
- Utilization of the PHQ-9 to Monitor Depression Symptoms for Adolescents and Adults.
- Depression Remission or Response for Adolescents and Adults
- Unhealthy Alcohol Use Screening and Follow-Up
- Pneumococcal Vaccination Coverage for Older Adults